Electroconvulsive therapy during pregnancy: a systematic review of case studies
Archives of Women’s Mental Health volume 18, pages1–39 (2015) View as PDF

Abstract
This study aims to explore practice, use, and risk of electroconvulsive therapy (ECT) in pregnancy. A systematic search was undertaken in the databases Medline, Embase, PsycINFO, SveMed and CINAHL (EBSCO). Only primary data-based studies reporting ECT undertaken during pregnancy were included. Two reviewers independently checked study titles and abstracts according to inclusion criteria and extracted detailed use, practice, and adverse effects data from full text retrieved articles. Studies and extracted data were sorted according to before and after year 1970, due to changes in ECT administration over time. A total of 67 case reports were included and studies from all continents represented. Altogether, 169 pregnant women were identified, treated during pregnancy with a mean number of 9.4 ECTs, at mean age of 29 years. Most women received ECT during the 2nd trimester and many were Para I. Main diagnostic indication in years 1970 to 2013 was Depression/Bipolar disorder (including psychotic depression). Missing data on fetus/child was 12 %. ECT parameter report was often sparse. Both bilateral and unilateral electrode placement was used and thiopental was the main anesthetic agent. Adverse events such as fetal heart rate reduction, uterine contractions, and premature labor (born between 29 and 37 gestation weeks) were reported for nearly one third (29 %). The overall child mortality rate was 7.1 %. Lethal outcomes for the fetus and/or baby had diverse associations. ECT during pregnancy is advised considered only as last resort treatment under very stringent diagnostic and clinical indications. Updated international guidelines are urgently needed.
Introduction
For patients with severe psychiatric disorders in the pregnancy period, either medication resistant illness, extremely high suicide risk, psychotic agitation, severe physical decline due to malnutrition or dehydration, electroconvulsive therapy (ECT) still appears as a strong option (Berle et al. 2011; 2003). Previous review publications have advocated ECT to be a relatively safe during pregnancy (Anderson and Reti 2009; Miller 1994; Reyes et al. 2011; Saatcioglu and Tomruk 2011). International ECT guidelines have no clear statements about pregnancy being a contraindication (American Psychiatric 2001; Enns et al. 2010; Royal College of Psychiatrists 2005). Checklists for when ECT is an option during pregnancy have also been provided in textbooks of interface between gynecology and psychiatry (Stewart and Erlick Robinson 2001), without mention of any potential risks to be taken into account.
Prevalence of major depressive episode (MME) during pregnancy is estimated at 12.4 % (Le et al. 2011). Considering that depression is the most common mental disorder (63 %), followed by bipolar disorder (43 %) and schizophrenia (13 %) among deliveries to women with atypical antipsychotic use (Toh et al. 2013), the decision of ECT during pregnancy would not appear uncommon. Although prevalence data on ECT administered during pregnancy is not retrievable, and ECT clearly rarely used during pregnancy in most clinical settings as illustrated by a recent review of contemporary use and practice of ECT worldwide (Leiknes et al. 2012), ECT was noted administered during pregnancy at 10 Polish sites (Gazdag et al. 2009) and also in Spain (Bertolin-Guillen et al. 2006).
Administration of psychotropic drugs during pregnancy requires great caution and benefits must be weighed against potential risks, especially in the first trimester (Stewart and Erlick Robinson 2001). Although evidence for psychotropic medication teratogenicity is generally lacking or limited (Gentile 2010), mood stabilizers such as lithium and valproate are strongly discouraged (Berle and Spigset 2003; Gentile 2010) and carbamazapine controversial (Gentile 2010; Stewart and Erlick Robinson 2001). As for antidepressants, a recent population-based cohort study data from the Danish Fertility Database has found no associated risk with use of SSRIs during pregnancy (Jimenez-Solem et al. 2013). For antipsychotics the risk associated with use during pregnancy is unclear (McCauley-Elsom et al. 2010).
In a systematic review concerning children of women with epilepsy (WWE), no support was found for the common view that epilepsy per se represented a risk for increased congenital malformations (Fried et al. 2004). Conversely, a large population-based register study found a twofold overall risk of malformation in the offspring from WWE compared with those without epilepsy (Artama et al. 2006). Caesarian section in WWE has, also been found to be performed twice as frequently compared with the general population (Olafsson et al. 1998). Total prevalence of major congenital anomalies, is by a large European study (Dolk et al. 2010) reported as 23.9 per 1,000 births for 2003–2007 and 80 % live births. Prevalence of congenital heart disease (the most common birth defect) to be 4–6/1,000 live births by another USA study (Ermis and Morales 2011).
In a previous review of the literature from 1941 to 2007 undertaken by Anderson and Reti (2009), with 57 included studies, ECT was reported administered to 339 women during pregnancy. The same review also reports a partial positive ECT response for pregnant women together with a very low number (N= 11) of ECT-related fetal or neonatal abnormalities. Whether these numbers can be reaffirmed and whether there is enough support for APAs the statement that ECT treatment has a “low risk and high efficacy in the management of specific disorders in all three trimesters of pregnancy” (American Psychiatric 2001) is a concern for this present review.
Treatment of mental disorders in pregnancy poses a unique clinical challenge due to potential effects also on the fetus from the intervention. As ECT is utilized worldwide and predominantly in the treatment of women (Leiknes et al. 2012), updated knowledge about safety and risk of ECT treatment during pregnancy for both the mother and fetus/child is of utmost primary importance.
Against this background, the main objective of this article is to give a systematic case overview of ECT administered during pregnancy, with newer date studies in mind, as well as to report the potential harm (adverse events for mother and fetus/baby).
Materials and methods
Data sources and search strategy
A systematic literature search was undertaken in the following databases: Ovid MEDLINE, Embase (Ovid) PsycINFO (Ovid), SveMed, Ovid Nursing Database and CINAHL (EBSCO) (Table 5 in Appendix 1) in September 2010. The search was updated in January and November 2012 and supplemented with ISI web of Knowledge, Clinical Trials.gov, PROSPERO (CRD), WHO ICTRP, POP-database (Table 6 in Appendix 1). Search terms intended for Medline were adapted (such) as required for the other databases. Subject headings and free text words used were “electroconvulsive therapy,” “electroshock,” “electroconvulsive,” “ECT,” combined with “pregnancy” or “pregnant women” and any of the following “antenatal,” “prenatal,” “perinatal,” “gravid,” or “gestation” limited to human studies and dating until today. The search did not exclude the postpartum period to make sure that no articles on the topic were missed. No date limitation was set to find all possible earliest published cases from the 1940s. Relevant references, known to authors of this review from earlier published reviews on this topic or reference lists in retrieved included papers, were also found by hand.
Inclusion and exclusion criteria
Inclusion criteria
Studies in the following languages were included: English, Norwegian, Swedish, Danish, Dutch, French, Italian, and Spanish. In addition to authors’ European language fluency, the online Google translation tool (http://translate.google.com/) was used when needed.
Exclusion criteria
Exclusion criteria include not a data-based study, no or unclear report of ECT undertaken during pregnancy, pseudocyesis, ECT undertaken only in the postpartum period, and not during pregnancy.
Screening of literature
Two reviewers (Kari Ann Leiknes (KAL) and Bjørg Høie (BH)) independently checked the titles, and where available, the abstracts of the studies identified by the electronic database searches. All references appearing to meet inclusion criteria, including those with insufficient details were requested in full text. Reviewers (KAL, BH, and Mary J. Cooke (MJC)), consisting of two pairs independently extracted data from the retrieved full-text articles according to a pre-designed data extraction scheme. All discrepancies were resolved by consensus meeting/discussion, and the final decision was made by the first author (KAL). Ingrid Harboe (IH) undertook the extensive updated literature search. All authors (including Lindy Jarosch-von Schweder (LJS) have contributed to the data presentation and manuscript text.
Data extraction
Briefly, the following aspects were considered: ECT practice and use; publication year and country; diagnoses/indication; mother’s age; number of pregnancies (primipara (P1), multipara (P2, 3), etc.); time ECT was administered according to number of gestation weeks (GW), 1st trimester (≤13 GW), 2nd trimester (14–26 GW), 3rd trimester (≥27 GW); total number ECTs administered, ECT administration frequency (two to three times week); ECT parameters (i.e., the manner in which ECT is applied: brief pulse or sine wave current, device type, electrode placement bilateral (BL) or unilateral (UL)); anesthesia type and monitoring (of both mother and fetus); time of birth; and adverse events mother (e.g., genital bleeding, miscarriage, eclampsia, and still birth) and/or baby (e.g., fetal malformations, Apgar score, etc.). As ECT treatment has changed over the years, as for use of anesthesia (termed modified ECT as opposed to unmodified ECT, without anesthesia), device and type of current (mainly from sine wave to brief pulse wave), a clinical cut off for presenting the extracted data was set at 1970.
Results
Study selection
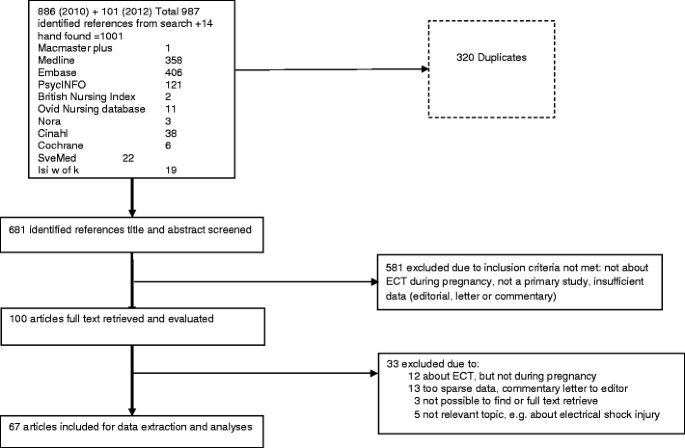
The study selection process, databases searched, and references identified are given in Fig. 1. Altogether, 1,001 references were identified: 681 titles and abstracts screened, 100 full texts screened, 67 included for data extraction, and 33 full texts excluded.
Description of studies
Overview of included case studies (N = 67) according to descending publication year, country represented, number of pregnancy cases and fetus and/or baby cases reported are given in Table 1. Overview of full text excluded studies (N = 33) and reasons for exclusion are given in Appendix 2. Twelve references were found not relevant to topic (about ECT, but not in pregnancy, e.g., in postpartum or other conditions), 13 had insufficient/too sparse data, 3 were impossible to find/full text retrieve, and 5 were not relevant, for example, only about anesthesia types or electrical shock accident injury during pregnancy. Detailed extracted data from each included study, such as diagnostic indication, ECT parameters, report of effect and events are presented in Summary of findings tables (N = 67), Appendix 3.Table 1 Overview of included studies (N = 67), publication year, country, number of pregnancy, and fetus/baby cases
A total of 67 case report studies were included, 42 (63 %) from 1970 to 2013 and 25 (37 %) from 1942 to 1970 (Table 1). The literature search included all years, but no studies according to inclusion criteria of this review were found in the 1970s (see Appendix 2 for two excluded 1970s studies (Levine and Frost 1975; Remick and Maurice 1978) lacking ECT data). Studies from all continents were represented as follows: North America (USA and Canada), 32; South America, 1; Europe, 25; Asia (including Middle East), 6; Africa, 2; and Australia, 1. A total of 169 pregnant women were ECT treated from 1942 to 2013. Reports on the fetus or newborn baby/child were found for only 148 cases resulting in 12 % “missing” fetus/baby data (see Table 1).
Altogether, 169 ECT treated pregnant women were identified, exposed to a total number of 1,187 ECTs. Mean and standard deviation (M (SD)) number of ECTs administered per pregnant woman was 9.4 (6.4). Mean age (M (SD) in years) of pregnant women treated with ECT was 28.9 (6.2) and age range 16½–48 years. Overview of ECT-treated pregnant women, number of ECTs, and diagnoses, after and before 1970 is given in Table 2.Table 2 ECT-treated pregnant women, number of ECTs, and diagnoses before and after 1970
Almost two thirds (63 %) diagnostic indication for ECT was Depression/Bipolar disorder (including psychotic depression) from year 1970 until today (2013), but Schizophrenia and other diagnoses the main indication (54 %) from 1942 until 1970 (Table 2). Diagnostic data was not missing in any reports from 1970 to 2013, but missing (15 %) and sometimes very unclear in several earlier reports from 1942 to 1970. Category of “other” diagnoses included obsessive–compulsive disorder (OCD) (Barten 1961; Fukuchi et al. 2003), generalized anxiety with panic attacks (Bhatia et al. 1999; Simon 1948), and Neuroleptic Malignant Syndrome (NMS) (Verwiel et al. 1994).
Altogether 21 out of 54 (39 %) women were nullipara (Para1) in the later years (from 1970 to 2013) (Table 2) and for one case in 2011 the pregnancy was by in vitro fertilization (Salzbrenner et al. 2011). The latest ECT administered in pregnancy was at 40 GW (Laird 1955; Schachter 1960) and the earliest at 4 GW (1955). Information about which pregnancy trimester the ECT was undertaken or started was found for 121 women out of 169 (28 % missing). Overview of the ECT reports according to pregnancy trimester for these 121 women is given in Table 3. Most women (53 %) received ECT during the 2nd trimester, although use in the 1st trimester was not uncommon (16 %) and for some, ECT was conducted throughout the entire pregnancy (Pinette et al. 2007).Table 3 ECT-treated women (N = 121) by pregnancy trimesters
Generally, the data reported in all studies was very varied concerning the ECT intervention per se, the setting of administration, monitoring, and outcome for both mother and fetus/child.
ECT practice during pregnancy
The setting in which the ECT was administered was usually not recorded. However, ECT undertaken in a surgical-obstetric recovery room or delivery environment was noted by three (Gilot et al. 1999; Wise et al. 1984; Yellowlees and Page 1990).
Monitoring of mother before, during, and after varied. In addition, monitoring of fetus varied greatly from some monitoring to no fetal monitoring by Vanelle et al. (1991). There was some use of cardiotocography (Molina et al. 2010; O’Reardon et al. 2011; Verwiel et al. 1994) but cardiotocography was also noted as not being useful in early pregnancy (before 24 GW) by Lovas et al. (2011). Mother in tilt position during ECT was used in some reports (Brown et al. 2003; Gilot et al. 1999; Livingston et al. 1994; Malhotra et al. 2008; Yang et al. 2011) and by others tilt position was reported not used (Bhatia et al. 1999; Bozkurt et al. 2007; DeBattista et al. 2003).
ECT parameters, such as electrical current type (brief pulse or sine wave), placement of electrodes (UL, BL, bitemporal, and bifrontal) and device manufacture type used was noted in most studies of later date but otherwise very sparsely. (See summary of findings table, Appendix 3). UL placement of electrodes was noted in six studies (Balki et al. 2006; Gahr et al. 2012; Pesiridou et al. 2010; Varan et al. 1985; Wise et al. 1984; Yellowlees and Page 1990).
Data on anesthetic agents used combined with muscle relaxant, premedication and 100 % oxygenation was mainly stated in the later date studies (1970 to 2013). Although 13 % of these later date studies (1970 to 2013) were missing anesthesia data, a trend was seen for the following being most used: thiopental (22 %), methohexital (15 %), and propofol (17 %). Anesthesia induced reduced fetal heart rate (FHR) was noted with propofol but not thiamylal in an ECT pregnancy case by Iwasaki et al. (2002). In addition, severe fetal bradycardia by methohexital but not with following propofol anesthesia during ECT administration by De Asis et al. (2013). To avoid pulmonary aspiration, tracheal intubation was preferred by Malhotra et al. (2008) when pregnancy was beyond 1st trimester.
Unmodified (without anesthesia) ECT was noted in the earlier studies (from 1942 to 1970), such as in all 8 cases reported by Laird (1955) and in 6 out of 15 cases by Smith (1956). Even use of only muscle relaxant without anesthesia was noted in 7 ECT pregnancy cases by Doan and Huston (1948).
Fetus, baby/child—monitoring, and follow-up
Fetus or baby/child data was sometimes totally absent even in the later date studies, such as in Gahr et al. (2012) and Ghanizadeh et al. (2009) as well as some earlier ones, for example Russell and Page (1955). Some reported new born baby Apgar score and weight, but most often the information on the newborn infant was meager and the condition of baby/child noted as normal, “healthy baby,” or nothing abnormal.
Information about monitoring of fetus during ECT varied greatly from none at all, to obstetric consultations and ultrasonography between treatment sessions (Espínola-Nadurille et al. 2007; Kasar et al. 2007; Serim et al. 2010) to before and after FHR and Doppler monitoring (O’Reardon et al. 2011).
Although most studies had no follow-up data on the children, some had sparsely noted follow-up at 1 month (Repke and Berger 1984), 3 months (Yellowlees and Page 1990), 18 months (O’Reardon et al. 2011), 2 weeks to 5 months (Sobel 1960), 2½ years (Yamamoto et al. 1953), and 6 years (Evrard 1961). A more detailed follow-up study from 1955 by Forssman (1955) of 16 children, whose mothers were given ECT during pregnancy between years 1947 and 1952, was excluded since it contained only data on the children without any ECT during pregnancy data on the mothers.
ECT risk and adverse events
No deaths of mother/ECT treated pregnant patient were found in any studies. Overall (all years), child mortality rate was 7.1 % (12/169), and from 1970 to 2013 mortality rate was 9.4 % (5/54) and from 1942 to 1970, 6.1 % (7/115) (see Table 1). Lethal outcomes for the fetus and/or baby were stated to have diverse causes, in one case a long lasting severe grand mal seizure (status epilepticus) induced by ECT (Balki et al. 2006). A combination of insulin coma treatment and ECT was found for 3 early studies in the period 1946 to 1954 by Kent (1947), Gralnick (1946), Wickes (1954)—all with severe very adverse outcome for the fetus/baby. Overview of all reported adverse events for ECT treated pregnant women and fetus and/or baby child are given in Table 4.Table 4 Overview of reported adverse events for ECT-treated pregnant women and fetus and/or baby found in all included (N = 67) studies
Report of adverse advents was high for both pregnant women and fetus/child in studies of later date period (1970 to 2013) compared with earlier date period (1942 to 1970) (see Table 4). Vaginal bleeding was reported more often during the 1st trimester, whereas uterine contractions, premature labour and caesarian sections occurred during 2nd and 3rd trimesters. The use of tocolytic treatment after ECT in order to avoid preterm labor was also noted by several (Fukuchi et al. 2003; Malhotra et al. 2008; Polster and Wisner 1999; Prieto Martin et al. 2006; Serim et al. 2010; Yang et al. 2011), as well as use of prophylactic tocolytic medication before ECT (Malhotra et al. 2008; Polster and Wisner 1999).
Discussion
Main findings
Altogether 169 ECT treated pregnant women of mean age 29 years, were identified. They were treated with mean number of ECTs 9.4, as treatment for mainly (62 %) severe “psychotic” depression/bipolar disorder. Half (53 %) of pregnant women received ECT during the 2nd trimester. ECT in the 1st trimester was not uncommon (16 %) and for some, ECT was conducted throughout the entire pregnancy. Altogether, 24 % women were nullipara (Para1). Fetus and/or baby report was found missing for 12 %. Child mortality rate was overall (all years) 7.1 %. A total of 67 adverse events were found among 169 women (rate, 0.40). Most common adverse event for mother was premature labor (born between 29 and 37 GW) 19/67 (28 %) and tocolytic treatment often noted. A total of 35 adverse events were found among the reported 148 fetus/baby children (rate 0.24). The most common reported adverse event for fetus/baby child occurring during the ECT intervention was reduced FHR 15/35 (43 %).
Whether the reduced FHR event is attributable to the ECT intervention per se or to the anesthetic agent or to both is not possible to say from such descriptive case studies. Due to the complexity of the ECT indication, the intervention per se, previous or concomitant psychotropic medication or other complicating somatic or genetic factors, direct causal inference is not possible to take from case studies. This being said though, having in mind that the risk of fetal malformation in WWE is twofold higher (Artama et al. 2006), and caesarian section performed more often among WWE (Olafsson et al. 1998), the potential risk involved with ECT induced epileptogenic seizures must in each case be considered. Such as illustrated in the recent publication by De Asis et al. (2013), where the ECT induced prolonged seizure duration occurred alongside severe reduced FHR and emergency Caesarian section prepared, but later abandoned when the FHR returned to normal. An earlier study (Balki et al. 2006) also reports severe ECT induced status epilepticus with lethal outcome for the fetus/child.
As for the overall occurrence of serious adverse events, such as stillbirth/neonatal death 8/35 (23 %) and fetal malformation 7/35 (20 %), the rates appear higher than that reported in the general population, i.e. 2.3 % major congenital abnormalities and 80 % live births (2010) and 0.6 % congenital heart disease (Ermis and Morales 2011). Some included studies though claim the miscarriage rate not to be higher than in the general population (Malhotra et al. 2008) and ECT to be less risky than pharmacological treatment (Kasar et al. 2007). However, figures from case studies cannot directly be compared with figures from large observational prevalence studies. This being said, close monitoring of mother and fetus during and after ECT treatment taking into regard the trimester situation, is crucial to bear in mind, such as use of cardiotocography, ultrasound between treatments, tilt position for mother including tocolytic treatment to prevent preterm labor. All these monitoring factors varied greatly in the included studies.
Direct effect of anesthetic agents on the fetus is still relatively unknown (Iwasaki et al. 2002). FHR variability and reduction under the ECT intervention is often mentioned as something to expect to happen. Propofol’s known associated risk of bradycardia calls for alertness from a fetal cardiovascular viewpoint and extra caution is needed where the fetus is immature or has cardiovascular complications. Thiopental (22 %), methohexital (15 %), and propofol (17 %) are the most used anesthetic agents. However, case studies with both anesthesia in favor of propofol (De Asis et al. 2013) and that against it (Iwasaki et al. 2002) are published.
Some factors to bear in mind in the different pregnancy trimesters are mentioned below:
- 1st trimesterKnowledge about when and how to administer ECT in early pregnancy, in order to reduce risk for both mother and fetus, is limited. Cardiotocography monitoring for the fetus, in this early period (before 24 GW) is not so feasible (Lovas et al. 2011). Risk of post ECT vaginal bleeding (indicative of abruptio placenta) and abortion (Vanelle et al. 1991) is mentioned. The complexity of any causal attribution to ECT is illustrated in the case by Yang (Yang et al. 2011) reporting congenital hyaline membrane disease and hypertrophic pyloric stenosis in a premature baby delivered by emergency section, since the mother had been treated with an extensive amount of antipsychotic and antidepressant medication prior to admission due to a 15 year long history of schizophrenia.
- 2nd trimesterTransient FHR reduction (bradycardia) arising during the ECT and subsiding afterwards is commonly reported from this trimester period, likewise post-ECT uterine contractions. The need for both pre- and post-ECT tocolytic treatment in order to avoid preterm labor is considerable (Fukuchi et al. 2003; Malhotra et al. 2008; Polster and Wisner 1999; Prieto Martin et al. 2006; Serim et al. 2010; Yang et al. 2011).
- 3rd trimesterTilt position is recommended by several, especially in the last trimester in order to reduce risk of gastric reflux. Also inhalation anesthesia is pointed out by Ishikawa et al. (2001) to be beneficial in the last stages of pregnancy in order to reduce uterine contraction and potential uterine relaxation effect of anesthetics.
The overall total number of included studies (N = 67) in our review is larger than the 57 by Anderson and Reti (2009). However, overall total number of ECT treated pregnant women (N = 169) is much less than the 339 by the same authors (Anderson and Reti 2009). Unlike the Anderson and Reti (2009), numbers of ECT treated pregnant women referred to by others in the general text of the case article, have not been included in this review. Strictly according to the predetermined review criteria, only direct case reports by the study authors are included in the total count number (169) of pregnant ECT treated women by us. For example, only one case is included in this review from the publication by Impastato et al. (1964) as opposed to 159 cases by Anderson and Reti (2009), and we have not included the Forssman (1955) follow-up of 16 infants/children on ECT treated mothers, since this study contains no ECT pregnancy data, i.e. data on the mothers treatment. Likewise the study by Levine and Frost (1975) is excluded by us, since it only contained information about anesthesia type and cardiovascular responses to ECT in a 3rd semester pregnancy and no other information.
Previous studies, such as that by O’Reardon et al. (2011) and previous reviews (Anderson and Reti 2009; Miller 1994; Saatcioglu and Tomruk 2011) as well as international guidelines (American Psychiatric 2001; Enns et al. 2010; Royal College of Psychiatrists 2005) and recent textbooks (Stewart and Erlick Robinson 2001) have regarded ECT to be relatively safe during all trimesters of pregnancy. Contrary to this standpoint, our review and overview of recorded adverse events from all case studies call for great clinical caution. Voices of concern, similar to ours, appear also in the included study Pinette et al. (2007) and APA statements regarding ECT as a safe intervention during pregnancy questioned. The previous held opinion by the Miller (1994) review concerning potential complications from ECT during pregnancy to be minimized by improved technique, are also questioned by our results.
Check lists
The study by Salzbrenner et al. (2011) provides a 10-point checklist for pregnant women undergoing ECT. Similarly, a 14-item list for general measures and routine anesthetic measures in order to avoid gastric reflux is provided by O’Reardon et al. (2011). The need for close clinical collaboration between gynecology/obstetrics, anesthesiology and psychiatry together with clear responsibility is evident. Textbook checklists for when ECT is an option during pregnancy (Stewart and Erlick Robinson 2001) need updating of potential risks to be considered.
Our results reveal that all potential risk arising from the complexity of ECT intervention, the grand mal seizure, anesthetic and concomitant or previous psychotropic medications, is of great concern and must be taken into account for both mother and fetus/child, and weighed against the clinical benefits, when deciding to administer ECT during pregnancy.
Ethical issues
Ethical considerations and possible ethical violations for both mother and the unborn non-consenting child are not discussed. Conflicting opinions can easily arise, such as that described by Polster and Wisner (1999) where the obstetrician advised that ECT be discontinued after premature labor treatment in the obstetrics unit, but ECT was continued by the psychiatric unit. All arguments from this review support the need for holistic clinical decision making and caution when ECT is considered as an option during pregnancy.
Strengths and limitations
The strength of this paper is the thorough, systematic review of all published literature without any data limitation. Data extracted from the included studies have strictly been limited to primary case presentations by the authors and not secondary “known to the authors” numbers referred to by the authors in the body text. Likewise all other literature review studies on the subject without any primary case data have also been excluded. The most consistent findings in all included studies was the number of ECTs administered, thereafter the diagnostic indication, pregnancy length, ECT parameters, anesthesia type, condition of both mother and child, the latter was somewhat more dependable in newer date studies. The strength of case study design is the reporting of rare and adverse events, however limitations as for this design must clearly be taken into account.
A limitation is uncertainty in the very oldest published cases, where case presentation is mixed with cases “known to authors” in the manuscript text, to completely document all cases since the introduction of ECT in 1938. The earliest published case reports are also much more likely to be mixed with other treatment forms, such as insulin coma, which is not used and out of date today and these mixed treatment reports therefore not so relevant for today’s practice. No prospective or controlled study design of ECT in pregnancy are found, case studies alone in this field provide the knowledge background. Case studies are susceptible to reporting and publication bias, and only descriptive aggregation of study data is possible, no meta-analyses. As cases of ECT during pregnancy where the treatment went well are most likely not published, the included studies in this review might very well be over represented with adverse event reporting.
Clinical implications
ECT during pregnancy should be a last resort treatment. For example in cases of severe depression, catatonia, medication resistant illness, extremely high suicide risk, psychotic agitation, severe physical decline due to malnutrition or dehydration or other life threatening conditions (for example malignant neuroleptic syndrome), where other treatment options are not possible or very inadequate. All potential risks of the ECT treatment, taking into account both mother and fetus, should be weighed against benefits. The ECT should be administered in a hospital emergency setting or delivery room. Information to patients of all possible risks involved should be considered compulsory. ECT during pregnancy should be administered by a highly skilled and competent specialist team consisting of psychiatrist, gynecologist/obstetrician, and anesthesiologist. Monitoring of patient under ECT treatment and also in the recovery room should include midwife and psychiatric nurse. The establishment of a multi-disciplinary specialist team bearing full treatment and follow-up responsibility is fundamental for the safety of the intervention.
Conclusions
Case reports on ECT administered during pregnancy provide vital knowledge. ECT during pregnancy is advised considered only under very stringent diagnostic and clinical indications, weighing all potential risks against benefits. Updated clinical guidelines are urgently needed in this field.
Abbreviations
BL:
BilateralBH:
Bjørg HøieBPM:
Beats (heart beats) per minuteDSM-IV:
Diagnostic Statistical Manual of Mental Disorders, fourth editionECT:
Electroconvulsive therapyEEG:
ElectroencephalogramFHR:
Fetal heart rateGW:
Gestation weeksICD-10:
International Classification of Diseases, 10th revisionIH:
Ingrid HarboeKAL:
Kari Ann LeiknesKTH:
Karianne Thune HammerstrømLJS:
Lindy Jarosch-von SchwederM:
MeanMJC:
Mary Jennifer CookeMRI:
Magnetic resonant imagingOCD:
Obsessive Compulsive DisorderSD:
Standard deviationUL:
UnilateralWWE:
Women with epilepsy
References
- American Psychiatric Association (2001). Weiner RD (ed). The practice of electroconvulsive therapy: recommendations for treatment, training, and privileging: a task force report of the American Psychiatric Association. The American Psychiatric Association, Washington, DC
- Anderson AJ (1968) The effects of electroconvulsive seizures during pregnancy on behavioral development of the offspring. DAI 29(6-B):2189Google Scholar
- Anderson EL, Reti IM (2009) ECT in pregnancy: a review of the literature from 1941 to 2007. Psychosom Med 71(2):235–242PubMed Google Scholar
- Anonymous (1997) Consult stat. Mom’s electric shock doesn’t affect the fetus. RN 60(10):79–80Google Scholar
- Artama M, Ritvanen A, Gissler M, Isojarvi J, Auvinen A (2006) Congenital structural anomalies in offspring of women with epilepsy: a population-based cohort study in Finland. Int J Epidemiol 35(2):280–287PubMed Google Scholar
- Bader A, Frisch U, Wirz-Justice A, Riecher-Rossler A (2010) Depression during pregnancy and its treatment. Nervenarzt 81(3):267–276CAS PubMed Google Scholar
- Balki M, Castro C, Ananthanarayan C (2006) Status epilepticus after electroconvulsive therapy in a pregnant patient. Int J Obstet Anesth J.(4):325–328
- Barten JJ (1961) Shock therapy during pregnancy. Ned Tijdschr Geneeskd 105:1142–1146CAS PubMed Google Scholar
- Berle JØ (1999) Severe postpartum depression and psychosis – when is electroconvulsive therapy the treatment of choice? Tidsskrift for den Norske LaegeforeningJF – Tidsskrift for den Norske Laegeforening 119(20):3000–3003CAS Google Scholar
- Berle JO, Spigset O (2003) Psychiatric disorders during pregnancy and lactation. Tidsskr Nor Laegeforen 123(15):2037–2040PubMed Google Scholar
- Berle JO, Solberg DK, Spigset O (2011) Treatment of bipolar disorder during pregnancy and in the postpartum period. Tidsskr Nor Laegeforen 131(2):126–129PubMed Google Scholar
- Bernardo M, Pintor L, Arrufat F, Salva J, Buisan E (1996) Delusion of pregnancy in psychotic depression and ECT response. Convuls Ther 12(1):39–40CAS PubMed Google Scholar
- Bertolin-Guillen JM, Peiro-Moreno S, Hernandez-de-Pablo ME (2006) Patterns of electroconvulsive therapy use in Spain. Eur Psychiatr 21(7):463–470Google Scholar
- Bhatia SC, Baldwin SA, Bhatia SK (1999) Electroconvulsive therapy during the third trimester of pregnancy. J ECT 15(4):270–274CAS PubMed Google Scholar
- Block S (1948) Electric convulsive therapy during pregnancy. Am J Psychiatry 104(8):579CAS PubMed Google Scholar
- Boyd DA, Brown DW (1948) Electric convulsive therapy in mental disorders associated with childbearing. Mo Med 45:573–579PubMed Google Scholar
- Bozkurt A, Karlidere T, Isintas M, Ozmenler NK, Ozsahin A, Yanarates O (2007) Acute and maintenance electroconvulsive therapy for treatment of psychotic depression in a pregnant patient. J ECT 23(3):185–187PubMed Google Scholar
- Brown NI, Mack PF, Mitera DM, Dhar P (2003) Use of the ProSeal laryngeal mask airway in a pregnant patient with a difficult airway during electroconvulsive therapy. Br J Anaesth 91(5):752–754PubMed Google Scholar
- Bruggeman R, de Waart MJ (1994) Successful electroconvulsive therapy in a pregnant woman with malignant neuroleptic syndrome. Ned Tijdschr Geneeskd 138(19):977CAS PubMed Google Scholar
- Ceccaldi P-F, Dubertret C, Keita H, Mandelbrot L (2008) Use of sismotherapy during pregnancy for severe depression. Gynecol Obstet Fertil 36(7–8):773–775PubMed Google Scholar
- Charatan FB, Oldham AJ (1954) Electroconvulsive treatment in pregnancy. J Obstet Gynaecol Br Emp 61(5):665–667CAS PubMed Google Scholar
- Cohn CK, Rosenblatt S, Faillace LA (1977) Capgras’ syndrome presenting as postpartum psychosis. South Med J 70(8):942CAS PubMed Google Scholar
- Cooper HH (1952) Electroshock treatment of mental illness during pregnancy. S Afr Med J Afr (17):366–368
- Cutajar P, Wilson D, Mukherjee T (1998) ECT used in depression following childbirth, in a woman with learning disabilities. Br J Learn Disabil 26(3):7Google Scholar
- De Asis SJ, Helgeson L, Ostroff R (2013) The use of Propofol to prevent fetal deceleration during electroconvulsive therapy treatment. J ECT (in press)
- DeBattista C, Cochran M, Barry JJ, Brock-Utne JG (2003) Fetal heart rate decelerations during ECT-induced seizures: is it important? Acta Anaesthesiol Scand 47(1):101–103CAS PubMed Google Scholar
- Doan DI, Huston PE (1948) Electric shock during pregnancy; a report of seven cases. Psychiatr Q 22(3):413–417CAS PubMed Google Scholar
- Dolk H, Loane M, Garne E (2010) The prevalence of congenital anomalies in Europe. Adv Exp Med Biol 686:349–364PubMed Google Scholar
- Dorn JB (1985) Case report: electroconvulsive therapy with fetal monitoring in a bipolar pregnant patient. Convuls Ther 1(3):217–221PubMed Google Scholar
- Echevarria MM, Martin MJ, Sanchez VJ, Vazquez GT (1998) Electroconvulsive therapy in the first trimester of pregnancy. J ECT 14(4):251–254Google Scholar
- Enns MW, Reiss JP, Chan P (2010) Electroconvulsive therapy. [Position Paper 1992-27-R1]. Can J Psychiatry 55(6):Insert, 1–12Google Scholar
- Ermis PR, Morales DL (2011) The adult Fontan patient: update for 2011. Methodist Debakey Cardiovasc J 7(2):3–8PubMed Google Scholar
- Eskes TK, Nijhuis JG (1994) Successful electroconvulsive therapy in a pregnant woman with malignant neuroleptic syndrome. Ned Tijdschr Geneeskd 138(19):976–977CAS PubMed Google Scholar
- Espínola-Nadurille M, Ramírez-Bermúdez J, Fricchione GL (2007) Pregnancy and malignant catatonia. Gen Hosp Psychiatry 29(1):69–71PubMed Google Scholar
- Evrard A (1961) Electroshock in pregnancy. Belg Tijdschr Geneesk 17:1136–1137CAS PubMed Google Scholar
- Ferrari B (1960) Electroshock in treatment of some psychoses of the pregnancy. Ann Ostet Ginecol 82:43–52Google Scholar
- Finnerty M, Levin Z, Miller LJ (1996) Acute manic episodes in pregnancy. Am J Psychiatry 153(2):261–263CAS PubMed Google Scholar
- Forman GW, Kearby HD, Grimes ME (1952) Electroshock therapy during pregnancy. Mo Med 49(9):773–775CAS PubMed Google Scholar
- Forssman H (1954) 16 Normally developed children whose mothers were treated with electroshock in pregnancy. Nord Med 52(44):1515CAS PubMed Google Scholar
- Forssman H (1955) Follow-up study of sixteen children whose mothers were given electric convulsive therapy during gestation. Acta Psychiatr Neurol Scand 30(3):437–441CAS PubMed Google Scholar
- Fried S, Kozer E, Nulman I, Einarson TR, Koren G (2004) Malformation rates in children of women with untreated epilepsy: a meta-analysis. Drug Saf 27(3):197–202PubMed Google Scholar
- Fukuchi T, Okada Y, Katayama H, Nishijima K, Kato S, Netsu S, Fukuda H (2003) A case of pregnant woman with severe obsessive-compulsive disorder successfully treated by modified-electroconvulsive therapy. Seishin Shinkeigaku Zassh 105(7):927–932Google Scholar
- Gahr M, Blacha C, Connemann BJ, Freudenmann RW, Schonfeldt-Lecuona C (2012) Successful treatment of major depression with electroconvulsive therapy in a pregnant patient with previous non-response to prefrontal rTMS. Pharmacopsychiatry 45(2):79–80CAS PubMed Google Scholar
- Gazdag G, Palinska D, Kloszewska I, Sobow T (2009) Electroconvulsive therapy practice in Poland. J ECT 25(1):34–38PubMed Google Scholar
- Gentile S (2010) Neurodevelopmental effects of prenatal exposure to psychotropic medications. Depress Anxiety 27(7):675–686PubMed Google Scholar
- Ghanizadeh A, Ghanizadeh MJ, Moini R, Ekramzadeh S (2009) Association of vaginal bleeding and electroconvulsive therapy use in pregnancy. J Obstet Gynaecol Res 35(3):569–571PubMed Google Scholar
- Gilot B, Gonzalez D, Bournazeau JA, Barriere A, Van Lieferinghen P (1999) Case report: electroconvulsive therapy during pregnancy. Encéphale 25(6):590–594CAS PubMed Google Scholar
- Ginsberg DL (2007) Neonatal brain infarcts possibly due to electroconvulsive therapy during pregnancy [Psychopharmacology reviews: October 2007]. Prim Psychiatry 14(10):20–21Google Scholar
- Gralnick A (1946) Shock therapy in psychoses complicated by pregnancy; report of two cases. Am J Psychiatry 102:780–782CAS PubMed Google Scholar
- Griffiths EJ, Lorenz RP, Baxter S, Talon NS (1989) Acute neurohumoral response to electroconvulsive therapy during pregnancy. A case report. J Reprod Med 34(11):907–911CAS PubMed Google Scholar
- Howe GB, Srinivasan M (1999) A case study on the successful management of Cotard’s syndrome in pregnancy. Int J Psychiatry Clin Pract 3(4):293–295CAS PubMed Google Scholar
- Impastato DJ, Gabriel AR (1957) Electroshock therapy during the puerperium. J Am Med Assoc 163(12):1017–1022CAS PubMed Google Scholar
- Impastato DJ, Gabriel AR, Lardaro HH (1964) Electric and insulin shock therapy during pregnancy. Dis Nerv Syst 25:542–546CAS PubMed Google Scholar
- Ishikawa T, Kawahara S, Saito T, Otsuka H, Kemmotsu O, Hirayama E, Ebina Y et al (2001) Anesthesia for electroconvulsive therapy during pregnancy – a case report. Masui 50(9):991–997CAS PubMed Google Scholar
- Iwasaki K, Sakamoto A, Hoshino T, Ogawa R (2002) Electroconvulsive therapy with thiamylal or propofol during pregnancy. Can J Anaesth 49(3):324–325PubMed Google Scholar
- Jimenez-Solem E, Andersen JT, Petersen M, Broedbaek K, Lander AR, Afzal S, Torp-Pedersen C et al (2013) SSRI Use During Pregnancy and Risk of Stillbirth and Neonatal Mortality. Am J Psychiatry 170(3):299–304PubMed Google Scholar
- Johnson I (1996) Steroid-induced prepartum psychosis. Br J Psychiatry 169(4):522CAS PubMed Google Scholar
- Kasar M, Saatcioglu O, Kutlar T (2007) Electroconvulsive therapy use in pregnancy. J ECT 23(3):183–184PubMed Google Scholar
- Kent EM (1947) Shock therapy during pregnancy. Psychiatr Q 21(1):102–106CAS PubMed Google Scholar
- Kramer BA (1990) Electroconvulsive therapy use during pregnancy. West J Med 152(1):77CAS PubMed Central PubMed Google Scholar
- Kucukgoncu S, Bestepe E, Calikusu C, Takmaz O, Tunc S, Erkoc S (2009) Clozapine and ECT treatment for pregnant woman with schizophrenia: A case report. Klin Psikofarmakol B 19(SUPPL. 1):S173-S175Google Scholar
- LaGrone D (1990) ECT in secondary mania, pregnancy, and sickle cell anemia. Convuls Ther 6(2):176–180PubMed Google Scholar
- Laird DM (1955) Convulsive therapy in psychoses accompanying pregnancy. N Engl J Med 252(22):934–936CAS PubMed Google Scholar
- Le SY, Dubertret C, Le FB (2011) Prevalence and correlates of major depressive episode in pregnant and postpartum women in the United States. J Affect Disord 135(1–3):128–138Google Scholar
- Leiknes KA, Jarosh-von SL, Hoie B (2012) Contemporary use and practice of electroconvulsive therapy worldwide. Brain Behav 2(3):283–344PubMed Central PubMed Google Scholar
- Levine R, Frost EA (1975) Arterial blood-gas analyses during electroconvulsive therapy in a parturient. Anesth Analg 54(2):203–205CAS PubMed Google Scholar
- Livingston JC, Johnstone WM Jr, Hadi HA (1994) Electroconvulsive therapy in a twin pregnancy: a case report. Am J Perinatol 11(2):116–118CAS PubMed Google Scholar
- Loke KH, Salleh R (1983) Electroconvulsive therapy for the acutely psychotic pregnant patient: a review of 3 cases. Med J Malays 38(2):131–133CAS Google Scholar
- Lovas A, Almos PZ, Peto Z, Must A, Horvath S (2011) Anesthesia for Electroconvulsive Therapy in Early Pregnancy. J ECT 27(4):328–330PubMed Google Scholar
- Maletzky BM (2004) The first-line use of electroconvulsive therapy in major affective disorders. J ECT 20(2):112–117PubMed Google Scholar
- Malhotra N, Vani, Malhotra P, Bhardwaj R (2008) Modified electroconvulsive therapy during pregnancy. J Anaesthesiol Clin Pharmacol 24(3):351–352Google Scholar
- Marcelino Da Silva L, Alexandre H (1950) Electroconvulsive therapy and pregnancy. J Bras Psiquiatr 1(7):91–96Google Scholar
- McCauley-Elsom K, Gurvich C, Elsom SJ, Kulkarni J (2010) Antipsychotics in pregnancy. J Psychiatr Ment Health Nurs 17(2):97–104CAS PubMed Google Scholar
- Miller LJ (1994) Use of electroconvulsive therapy during pregnancy. Hosp Community Psychiatry 45(5):444–450CAS PubMed Google Scholar
- Molina M, Vega O, Valero J, Rubio J, Povo A, Diago V, Perales A (2010) Electroconvulsive therapy during pregnancy. J Matern Fetal Neonatal Med(var.pagings):539
- Monod H (1955) Electric shock and pregnancy. Bull Fed Soc Gynecol Obstet Lang Fr 7(3):287–292CAS PubMed Google Scholar
- Mynors-Wallis LM (1989) Caution about sorcery. Br J Psychiatry 155:570, OctCAS PubMed Google Scholar
- Nielsen RE, Stage KB, Christensen PM, Mortensen S, Andersen LL, Damkier P (2007) Medical treatment of depression during pregnancy and breastfeeding [Danish]. Ugeskr Laeger 169(16):1442–1444PubMed Google Scholar
- Olafsson E, Hallgrimsson JT, Hauser WA, Ludvigsson P, Gudmundsson G (1998) Pregnancies of women with epilepsy: a population-based study in Iceland. Epilepsia 39(8):887–892CAS PubMed Google Scholar
- O’Reardon JP, Cristancho MA, Von Andreae CV, Cristancho P, Weiss D (2011) Acute and maintenance electroconvulsive therapy for treatment of severe major depression during the second and third trimesters of pregnancy with infant follow-up to 18 months: case report and review of the literature. J ECT 27(1):e23–e26PubMed Google Scholar
- Passov V (2010) Use of electro convulsive therapy for treatment resistant major depressive disorder in pregnant patients: case series [18th European Congress of Psychiatry]. Eur Psychiatry 25(Supp.1):1407Google Scholar
- Pesiridou A, Baquero G, Cristancho P, Wakil L, Altinay M, Kim D, O’Reardon JP (2010) A case of delayed onset of threatened premature labor in association with electroconvulsive therapy in the third trimester of pregnancy. J ECT 26(3):228–230PubMed Google Scholar
- Pinette MG, Wax JR (2010) The management of depression during pregnancy: a report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Obstet Gynecol 115(1):188–189PubMed Google Scholar
- Pinette MG, Santarpio C, Wax JR, Blackstone J (2007) Electroconvulsive therapy in pregnancy. Obstet Gynecol 110(2 II):465–466PubMed Google Scholar
- Plenter AM (1948) Electroshock therapy in pregnancy [Dutch]. Ned Tijdschr Geneeskd 92(15):1079–1082CAS PubMed Google Scholar
- Polatin P and Hoch P (1945) Electroshock therapy in pregnant mental patients. N Y State J Med:1562–1563.
- Polster DS, Wisner KL (1999) ECT-induced premature labor: a case report. J Clin Psychiatry 60(1):53–54CAS PubMed Google Scholar
- Porot M (1949) Psychiatric shock treatments and pregnancy [French]. Presse Med 57(76):1118–1120CAS PubMed Google Scholar
- Prieto Martin RM, Palomero Rodriguez MA, de Miguel FP, Yusta MG, Alonso BB, Muriel VC (2006) Electroconvulsive therapy in the third trimester of pregnancy: a case report [Spanish]. Rev Esp Anestesiol Reanim 53(10):653–656CAS PubMed Google Scholar
- Protheroe C (1969) Puerperal psychoses: a long term study: 1927–1961. Br J Psychiatry 115(518):9–30CAS PubMed Google Scholar
- Ratan DA, Friedman T (1997) Capgras syndrome in postpartum depression. Ir J Psychol Med 14(3):117–118Google Scholar
- Raty-Vohsen D (1982) Postpartum psychoses. Acta Psychiatr Belg 82(6):596–616CAS PubMed Google Scholar
- Remick RA, Maurice WL (1978) ECT in pregnancy. Am J Psychiatry 135(6):761–762CAS PubMed Google Scholar
- Repke JT, Berger NG (1984) Electroconvulsive therapy in pregnancy. Obstet Gynecol 63(3:Suppl):39S–41SCAS PubMed Google Scholar
- Reyes CB, Pena CH, Prieto MB, Llovera NF (2011) A systematic review of the use of ECT in pregnant women. Int Clin Psychopharmacol 26:e36–e37Google Scholar
- Richards DS (2007) Is electroconvulsive therapy in pregnancy safe? Obstet Gynecol 110(2 II):451–452PubMed Google Scholar
- Royal College of Psychiatrists (2005) The ECT handbook: the third report of the Royal College of Psychiatrist’s Special Committee on ECT. Royal College of Psychiatrists, LondonGoogle Scholar
- Russell RJ, Page LGM (1955) E.C.T in pregnancy. BMJ 1:1157PubMed Central Google Scholar
- Saatcioglu O, Tomruk NB (2011) The use of electroconvulsive therapy in pregnancy: a review. Isr J Psychiatry Relat Sci 48(1):6–11PubMed Google Scholar
- Salzbrenner S, Breeden A, Jarvis S, Rodriguez W (2011) A 48-year-old woman primigravid via in vitro fertilization with severe bipolar depression and preeclampsia treated successfully with electroconvulsive therapy. J ECT 27(1):e1–e3PubMed Google Scholar
- Schachter M (1960) Electric shock therapy during pregnancy and embryopathy. Electro-traumatic or viral embryopathy? Apropos of a clinical observation. Acta Paedopsychiatr 27:289–292CAS PubMed Google Scholar
- Serim B, Ulas H, Ozerdem A, Alkin T (2010) Electroconvulsive therapy in an adolescent pregnant patient. Prog Neuropsychopharmacol Biol Psychiatry 34(3):546–547PubMed Google Scholar
- Sherer DM, D’Amico ML, Warshal DP, Stern RA, Grunert HF, Abramowicz JS (1991) Recurrent mild abruptio placentae occurring immediately after repeated electroconvulsive therapy in pregnancy. Am J Obstet Gynecol 165(3):652–653CAS PubMed Google Scholar
- Simon JL (1948) Electric shock treatment in advanced pregnancy. J Nerv Ment Dis 107(6):579CAS PubMed Google Scholar
- Smith S (1956) The use of electroplexy (E.C.T.) in psychiatric syndromes complicating pregnancy. J Ment Sci 102(429):796–800CAS PubMed Google Scholar
- Sneddon J and Kerry RJ (1984) Puerperal psychosis: A suggested treatment model. American Journal of Social Psychiatry Vol 4(4), Fal 1984, pp 30-34(4):Fal-34Google Scholar
- Sobel DE (1960) Fetal damage due to ECT, insulin coma, chlorpromazine, or reserpine. AMA Arch Gen Psychiatr 2:606–611CAS Google Scholar
- Stewart DE and Erlick Robinson G (2001) Psychotropic drugs and electroconvulsive therapy during pregnancy and lactation (pp.67-93). In: Stotland NL and Stewart DE (eds) Psychological aspects of women’s health care: The interface between psychiatry and obstetrics and gynecology. xviii, 654 pp, 2nd. American Psychiatric Press, Inc, Washington, DC
- Stone CP, Walker AH (1949) Note on modification of effects of electroconvulsive shocks on maternal behavior by ether anesthesia. J Comp Physiol Psychol 42(5):429–432CAS PubMed Google Scholar
- Thorpe FT (1942) Shock Treatment in Psychosis complicating Pregnancy. Br Med J 2(4261):281CAS PubMed Central PubMed Google Scholar
- Toh S, Li Q, Cheetham TC, Cooper WO, Davis RL, Dublin S, Hammad TA et al (2013) Prevalence and trends in the use of antipsychotic medications during pregnancy in the U.S., 2001–2007: a population-based study of 585,615 deliveries. Arch Womens Ment Health 16(2):149–157PubMed Central PubMed Google Scholar
- Vanelle JM, Bouvet O, Brochier P, Allouche G, Rouillon F, Loo H (1991) Role of electroshock therapy in puerperal mental disorders. Ann Med Psychol (Paris) 149(3):265–269CAS Google Scholar
- Varan LR, Gillieson MS, Skene DS, Sarwer-Foner GJ (1985) ECT in an acutely psychotic pregnant woman with actively aggressive (homicidal) impulses. Can J Psychiatr Rev Can Psychiatr 30(5):363–367CAS Google Scholar
- Verwiel JM, Verwey B, Heinis C, Thies JE, Bosch FH (1994) Successful electroconvulsive therapy in a pregnant woman with neuroleptic malignant syndrome. Ned Tijdschr Geneeskd 138(4):196–199CAS PubMed Google Scholar
- Walker R (1992) ECT and twin pregnancy. Convuls Ther 8(2):131–136PubMed Google Scholar
- Wickes IG (1954) Foetal defects following insulin coma therapy in early pregnancy. Br Med J 2(4845):1029–1030CAS PubMed Central PubMed Google Scholar
- Wise MG, Ward SC, Townsend-Parchman W, Gilstrap LC III, Hauth JC (1984) Case report of ECT during high-risk pregnancy. Am J Psychiatry 141(1):99–101CAS PubMed Google Scholar
- Yamamoto J, Hammes EM, Hammes EMJ (1953) Mental deficiency in a child whose mother was given electric convulsive therapy during gestation: a case report. Minn Med 36(12):1260–1261CAS PubMed Google Scholar
- Yang HS, Seo HJ, Lee YK (2011) Anesthetic care for electroconvulsive therapy during pregnancy. Korean J Anesthesiol 60(3):217–220PubMed Central PubMed Google Scholar
- Yellowlees PM, Page T (1990) Safe use of electroconvulsive therapy in pregnancy. Med J Aust 153(11–12):679–680CAS PubMed Google Scholar
- Yoong AF (1990) Electrical shock sustained in pregnancy followed by placental abruption. Postgrad Med J 66(777):563–564CAS PubMed Central PubMed Google Scholar
Acknowledgments
This study has been possible because of research commissioning on the topic “ECT for depression” from the Norwegian Directorate of Health to the Norwegian Knowledge Centre. We thank the Norwegian Knowledge Centre’s research librarian Karianne Thune Hammerstrøm (KTH) for designing and undertaking the first primary literature search.
Competing interests
None.
Funding statement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
- Norwegian Knowledge Centre for the Health Services, Box 7004 St. Olavsplass, Pilestredet Park 7, Oslo, 0130, NorwayKari Ann Leiknes, Ingrid Harboe & Bjørg Høie
- Department for Psychosis, Psychiatric Clinic, Haukeland University Hospital, Bergen, 5021, NorwayMary Jennifer Cooke
- Division of Psychiatry, Tiller DPS and Faculty of Medicine, Institute of Neuroscience, St. Olav’s University Hospital and Norwegian University of Science and Technology (NTNU), P O Box 3008, Lade, 7441, Trondheim, NorwayLindy Jarosch-von Schweder
Corresponding author
Additional information
Work conducted at: The Norwegian Knowledge Centre for the Health Services
Appendices
Appendix 1
Table 5 Search strategy in 2010
Full size tableTable 6 Search strategy, update in 2012
Appendix 2
Table 7 Excluded studies (N = 33)
Appendix 3
Table 8 Summary of findings tables of included case studies N = 67 (sorted descending by year)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Leiknes, K.A., Cooke, M.J., Jarosch-von Schweder, L. et al. Electroconvulsive therapy during pregnancy: a systematic review of case studies. Arch Womens Ment Health 18, 1–39 (2015). https://doi.org/10.1007/s00737-013-0389-0
- Received29 April 2013
- Accepted20 October 2013
- Published24 November 2013
- Issue DateFebruary 2015
- DOIhttps://doi.org/10.1007/s00737-013-0389-0



